
Dr. Fahad Alkherayf is the Director of the Clinical Research Program in the Neurosurgery Division of The Ottawa Hospital. As a neurosurgeon, he specializes in minimally invasive surgeries, which use much smaller incisions than traditional surgeriesLink opens in a new window. As a result, they can mean less pain, lower chance of infection, and quicker recovery time. As part of a highly skilled team at The Ottawa Hospital, Dr. Alkherayf is broadening the horizons in neurosurgery treatment and research — not just in Ottawa, but across Canada.
Q: How did you decide to go into the field of neurosurgery?
A: In my Grade 7 science class, we learned about the human body and how all the systems function together. It really started my interest in medicine, especially the brain. There were three of us in that class who were very close friends, and we shared this interest. All three of us became doctors: one is a psychiatrist, one a radiation oncologist. I went to medical school based on this, and during my schooling I spent time in neurosurgery and realized this would be my future.
Q: What have you learned since becoming a neurosurgeon?
A: I have learned that despite what the textbooks show and say about the brain, in real life each patient is unique, and what works for one patient might not work for another. This has inspired me to individualize each of my patients’ care.
Neurosurgery is also evolving at a fast pace, and a lot of the equipment we now use was not invented or used when I started in the field. A lot of historical neurosurgical procedures have been replaced with modern techniques.
Q: You used minimally invasive surgeryLink opens in a new window to remove a meningioma tumour from behind Michele Juma’s eyeLink opens in a new window. How did these new techniques help her?
A: Michele came to see me almost blind because the tumour was attached to her optic nerve. Identifying the margin between the tumour and the nerve without causing damage to her nerve was one of the biggest challenges in her surgery.
This type of tumour is not new, the presentation is not new, but the treatment is relatively new. We used to do craniotomies, which involve a big incision in the skin. You need to remove part of the skull, go underneath the brain, lift the brain up, and then work all the way to the centre and remove the tumour, aiming not to injure any of the structures around it. The challenge with that is it’s a long path, and it’s through a really big incision. We know with these, there is a higher risk of inuring the optic nerve.
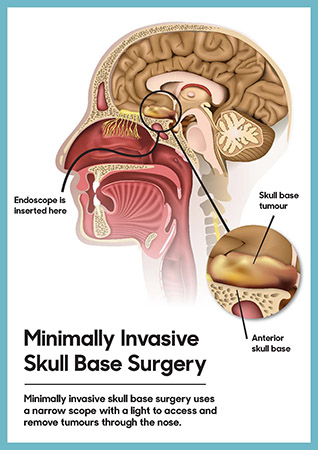
With patients like Michele, now instead of going through the old, traditional way — going through the scope, and lifting the brain up — we go through the nose.
Q: You also use a unique technique you call “vision monitoringLink opens in a new window” during certain minimally invasive surgeriesLink opens in a new window like Michele’s. Can you talk about that and what else The Ottawa Hospital is doing in neurosurgery that is exciting or groundbreaking?

A: The vision monitoring is teamwork where a neurophysiologist continuously monitors any changes in the patient’s vision during the surgery. This technique is done by applying goggles — similar to swimming goggles — over the patient’s eyes, which send signals through their eyes, and then we record the response from the patient’s vision centre. This allows the neurophysiologist to monitor any changes to the patient’s vision happening during the surgery. This live feedback helps the surgeon to achieve maximum resection (or removal) of tumours while minimizing the risk of injury to the visual pathway.
I am proud that this technique was significantly modified by our team here at The Ottawa Hospital. In addition to this unique technique, at The Ottawa Hospital we have advanced equipment including 3D endoscopes, along with techniques to inject the tumour with certain dyes to allow the tumour to be better visualized during the surgery.
Q: The Ottawa Hospital is currently working towards the creation of a new, world-class health and research centreLink opens in a new window to replace the aging Civic Campus. How will this new hospital campusLink opens in a new window, which will be the most technologically-advanced facility in Canada, make a difference for our neuro patients?
A: The new Civic Hospital will have the state-of-the-art technology that will advance the focus on individualized patient care.
The “one-model-fits-all” approach is changing in neurosurgery. Current research is focussing on individualized patient care. I see a future where each patient will have their surgery planned specific to their situation and needs — where artificial intelligence techniques would be part of planning for patient surgery.
Q: Why did you choose to work at The Ottawa Hospital instead of a different hospital?
A: One of the biggest advantages of The Ottawa Hospital is that all of us are connected. What happened in Michele’s case, for example, is that everything could go very quickly, because we are all in one centre. We are more advanced because we’re able to work as a group. We have brought all the expertise under one umbrella here.
I am a strong believer that the key thing for success is having a collaborative and supportive work environment. Of the many offers I received early in my career, The Ottawa Hospital, together with The Ottawa Hospital Research Institute, were the right fit for me. This kind of workplace, and the great city of Ottawa, was the best decision for my family.
Q: Where would we find you outside of work?
A: Depending on the time of year, you can find me playing soccer, hiking, camping with the kids, or taking care of the garden.
Q: What is something about you people might not know?
A: I have arachnophobia.

