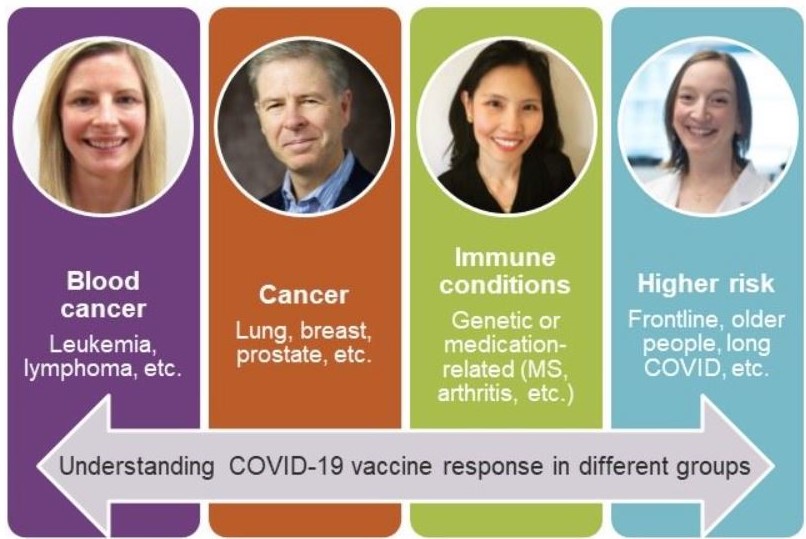
 Four new studies will answer important questions about how different groups respond to COVID-19 vaccines. From left to right, Dr. Arianne Buchan is leading a study in people with blood cancer, Dr. Glenwood Goss is leading a study in people with other kinds of cancer, Dr. Juthaporn Cowan is leading a study in people with immune conditions and Dr. Angela Crawley is leading a study in higher risk occupations and in which effects of age and "long COVID" will be examined.Researchers at The Ottawa Hospital and the University of Ottawa have been awarded more than $8 million to lead four national studies that will answer important questions about COVID-19 vaccines, including how well they work in people with cancer and immune conditions and in our aging population.
Four new studies will answer important questions about how different groups respond to COVID-19 vaccines. From left to right, Dr. Arianne Buchan is leading a study in people with blood cancer, Dr. Glenwood Goss is leading a study in people with other kinds of cancer, Dr. Juthaporn Cowan is leading a study in people with immune conditions and Dr. Angela Crawley is leading a study in higher risk occupations and in which effects of age and "long COVID" will be examined.Researchers at The Ottawa Hospital and the University of Ottawa have been awarded more than $8 million to lead four national studies that will answer important questions about COVID-19 vaccines, including how well they work in people with cancer and immune conditions and in our aging population.
The Government of Canada is funding the projects through its COVID-19 Immunity Task Force and Vaccine Surveillance Reference Group (VSRG).
“Our researchers are making crucial contributions to the global fight against COVID-19,” said Dr. Duncan Stewart, Executive Vice-President of Research at The Ottawa Hospital and professor at the University of Ottawa. “These new studies will help us protect some of our most vulnerable populations and advance vaccine science worldwide.”
How well do COVID-19 vaccines work in people with blood cancer?
Blood cancer, and the treatments used to fight it, can weaken the immune system and make patients more susceptible to viruses like COVID-19. A weak immune system can also mean a weaker response to vaccines, but very little research has been done on COVID-19 vaccines in people with blood cancer.
Dr. Arianne Buchan, an infectious disease specialist and clinician investigator at The Ottawa Hospital and assistant professor at the University of Ottawa, is leading a national study to determine how well COVID-19 vaccines work in people with blood cancer. The study aims to recruit 1,400 people from more than a dozen hospitals across the country, with coordinating centres in Ottawa, Edmonton, Montreal and Toronto.
The team is recruiting participants with leukemia, lymphoma, myeloma and other kinds of blood cancer, including those who have undergone stem cell transplantation. Both unvaccinated and vaccinated people can participate. Participants will be asked to provide blood samples and fill out questionnaires.
The researchers will measure the body’s immune response to COVID-19 vaccines and track if participants develop COVID-19 over the “People with blood cancers have higher risk of severe illness with COVID-19 infection,” said Dr. Arianne Buchan. “Our study will provide data to help understand how our patients respond to COVID-19 vaccines and will help us protect them from infection moving forward.” course of the study.
“People with blood cancers have higher risk of severe illness with COVID-19 infection,” said Dr. Arianne Buchan. “Our study will provide data to help understand how our patients respond to COVID-19 vaccines and will help us protect them from infection moving forward.” course of the study.
“People with blood cancers have higher risk of severe illness with COVID-19 infection,” said Dr. Buchan. “Our study will provide data to help understand how our patients respond to COVID-19 vaccines and will help us protect them from infection moving forward.”
The study was awarded $2.1 million from the Government of Canada through its COVID-19 Immunity Task Force.
Co-Principal Investigators: Michael Sebag, Abi Vijenthira, Sita Bhella, Peng Wang
Co-Investigators: Lisa Hicks, Matthew Cheung, Curtis Cooper, Donna Reece, Joseph Brandwein, Michael Chu, Marc-André Langlois, Angela Crawley, David Allan, Natasha Kekre, Christopher Bredeson, Arleigh McCurdy, Andrew Aw, Vikas Gupta, Anca Prica, Stephen Betschel, Grame Fraser, Annette Hay, Joy Mangel, Anne-Claude Gingras, Deepali Kumar, Sasan Hosseini, Sarit Assouline, Anna Nikonova, Tony Reiman, Catherine Moltzan, Julie Stakiw, Carolyn Owen, Laurie Sehn, Shelly Bolotin, James Brooks
Partner institutions: McGill University Health Centre, University Health Network, University of Alberta, St. Michael’s Hospital, Sunnybrook Health Sciences Centre, Kingston Health Sciences Centre, London Health Sciences Centre, Lunenfeld-Tanenbaum Research Institute, Jewish General Hospital, Public Health Agency of Canada, Ottawa Methods Centre
For more information and to enroll:
How well do COVID-19 vaccines work in people with cancer?
Research is urgently needed to know how well COVID-19 vaccines work in people with cancer. More than 2 million Canadians are currently living with cancer and many of these individuals have weakened immune systems, either due to the cancer itself, or due to treatments such as radiation and chemotherapy.
The Ottawa Hospital and BC Cancer are leading a national study to address this knowledge gap, in partnership with Public Health Ontario and the BC Centre for Disease Control.
The study will enroll 300 adults with cancer in Ottawa and Vancouver, as well as 150 healthy volunteers in Ottawa. People with many kinds of cancer (e.g. lung, breast, prostate, colon and other solid tumours) can participate.
Blood samples will be collected at various time points after vaccination to measure vaccine-induced immune responses. The researchers will also look at antibody production, how well the antibodies neutralize the virus, and how well the cells of the immune system recognize the virus and develop lasting immunity. Where possible, this data will be combined with clinical outcomes of vaccine effectiveness, such as whether patients become infected with the virus after receiving the vaccine. “This Canadian-led study will determine if people with cancer can mount an appropriate immune response to COVID-19 vaccines,” said overall study lead Dr. Glenwood Goss. “It will provide critical information to patients, health care providers, public health authorities and regulatory agencies.”
“This Canadian-led study will determine if people with cancer can mount an appropriate immune response to COVID-19 vaccines,” said overall study lead Dr. Glenwood Goss. “It will provide critical information to patients, health care providers, public health authorities and regulatory agencies.”
“This Canadian-led study will determine if people with cancer can mount an appropriate immune response to COVID-19 vaccines,” said overall study lead Dr. Glenwood Goss, who is a medical oncologist and senior clinician investigator at The Ottawa Hospital and professor at the University of Ottawa. “It will provide critical information to patients, health care providers, public health authorities and regulatory agencies.”
The study was awarded $1.9 million from the Government of Canada through its COVID-19 Immunity Task Force.
Co-Principal Investigator: Stephen Chia
Co-Investigators: Carolina Ilkow, Diane Lu, Muhammad Morshed, Tim Ramsay, Manish Sadarangani, Inna Sekirov, Theodore Steiner
Partner institutions: The Ottawa Hospital, Ottawa Methods Centre, BC Cancer, University of British Columbia, Public Health Ontario, BC Centre for Disease Control, Public Health Agency of Canada
For more information and to enroll: etudeC19study@ohri.ca; 613-737-7700 x79767.
How well do COVID-19 vaccines work in people with inherited and medication-related immune deficiencies?
People with inherited immune deficiencies have a greater risk of developing severe COVID-19 and may be less likely to respond to vaccines. People with multiple sclerosis, arthritis and other immune-mediated diseases may also be at risk because medications for these conditions often suppress the immune system.
Dr. Juthaporn Cowan, infectious disease physician and associate scientist at The Ottawa Hospital and assistant professor at the University of Ottawa, is leading a national study to investigate how people with these conditions respond to COVID-19 vaccines.
The research team aims to recruit 460 participants with inherited or medication-related immune deficiencies from twelve sites across Canada (in Ottawa, Montreal, Toronto, Halifax, Winnipeg, Edmonton, Calgary and Vancouver). Participants must be at least 12 years old and must be either planning to get vaccinated or already vaccinated (up to 24 weeks post second dose).
The researchers also hope to recruit healthy individuals over 12 who have not yet been vaccinated, but plan to be, as a control group.
The researchers will collect blood samples from the participants to study the body’s response to COVID-19 vaccines, including antibody levels and T cell response. Participants will also fill out questionnaires and be followed by health care professionals to assess any vaccine side effects.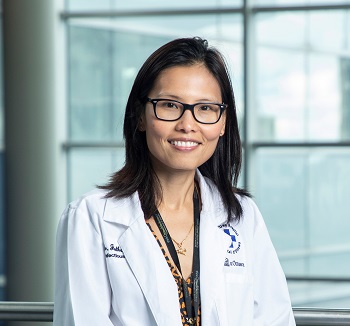 “Our study will provide crucial data to help us protect people with immune deficiencies against COVID-19,” said Dr. Juthaporn Cowan. “It will also help us learn more about which compartment of the immune system is essential in the COVID-19 vaccine response, so that better vaccines can be developed in future.”
“Our study will provide crucial data to help us protect people with immune deficiencies against COVID-19,” said Dr. Juthaporn Cowan. “It will also help us learn more about which compartment of the immune system is essential in the COVID-19 vaccine response, so that better vaccines can be developed in future.”
“Our study will provide crucial data to help us protect people with immune deficiencies against COVID-19,” said Dr. Cowan. “It will also help us learn more about which compartment of the immune system is essential in the COVID-19 vaccine response, so that better vaccines can be developed in future.”
The study was awarded $2.5 million from the Government of Canada through its COVID-19 Immunity Task Force.
Co-Principal Investigators: Donald C. Vinh, Emilia Liana Falcone, Hugo Chapdelaine
Co-Investigators: C. Arianne Buchan, Anne Pham-Huy, Marc-Andre Langlois, Tim Ramsay, Karina Top, Gina Lacuesta, Lisa Barrett, Beata Derfalvi, Alejandro Palma, Thomas Issekutz, Elie Haddad, Helene Decaluwe, Stephen Betschel, Julia Upton, Karver Zanorniak, Vy Hong-Diep Kim, Tamar Rubin, Lana Rosenfield, Chrystyna Kalicinsky, Colin Barber, Sneha Suresh, Mohammed Osman, Bruce Ritchie, Luis Murguia Favela, Nicola Wright, Manish Sadarangani, Kyla Hildebrand, Persia Poushahnazari, Fabien Touzot
Partner institutions: Canadian Immunodeficiency Patient Organization, Canada Special Immunization Clinic Network, Multiple Sclerosis Society, Ottawa Methods Centre, Montreal Clinical Research Institute, University of Montreal, Dalhousie University, CHU Sainte-Justine, St. Michael’s Hospital, SickKids Hospital, University of Manitoba, University of Alberta, University of Calgary, University of British Columbia
Study website: https://omc.ohri.ca/VISID
How long does COVID-19 immunity last and how can we enhance protection for everyone?
What is a protective immune response to natural SARS-CoV-2 infection? Does it differ from that induced by vaccination? How many vaccine doses are needed? How long does immunity last? Can natural or vaccine immunity protect against infection by viral variants of concern? Is this protection as strong and of the same quality in the elderly, in COVID “long-haulers”, and in the immunocompromised? Does previous exposure to other seasonal coronaviruses influence immune responses to SARS-CoV-2?
Researchers from The Ottawa Hospital and the University of Ottawa, and their partners at McGill University and the National Research Council of Canada have been awarded more than $1.7 million to answer these questions through an expansion of the Stop the Spread Ottawa study.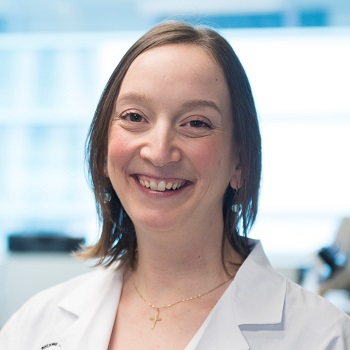 “This study will provide crucial information about the immune response to COVID-19 and to vaccines,” said Dr. Angela Crawley. “The results could help us end this pandemic sooner and maintain protective immunity, and also ensure that we are better prepared for possible future pandemics.”
“This study will provide crucial information about the immune response to COVID-19 and to vaccines,” said Dr. Angela Crawley. “The results could help us end this pandemic sooner and maintain protective immunity, and also ensure that we are better prepared for possible future pandemics.”
Dr. Angela Crawley, a scientist at The Ottawa Hospital and assistant professor at the University of Ottawa, is leading the expansion, with the original study led by the University of Ottawa’s Dr. Marc-André Langlois.
Launched in October 2020, Stop the Spread Ottawa has already recruited more than 1,000 participants who have either tested positive for SARS-CoV-2, or who have a higher risk of exposure. By collecting blood and saliva samples on a monthly basis since Oct 2020, the researchers have been able to gather valuable data about the immune response to SARS-CoV-2 infection, and as people are vaccinated. The cohort includes many front-line workers and patient subgroups of interest to the pandemic.
The new funding from the Government of Canada, through the COVID-19 Immunity Task Force, will allow the research team to expand the study to evaluate how immune cells called T cells respond to COVID-19, as well as antibodies and follow participants into 2022.
“This study will provide crucial information about the immune response to COVID-19 and to vaccines,” said Dr. Crawley. “The results could help us end this pandemic sooner and maintain protective immunity, and also ensure that we are better prepared for possible future pandemics.”
Stop the Spread Ottawa has also partnered with the new Coronavirus Variant Rapid Response Network, which was recently awarded $9 million from the Canadian Institutes of Health Research. Dr. Crawley is the Biobank Director for this study.
Collaborators: Angela Crawley, Marc-Andre Langlois, Steffany Bennett, Miroslava Culf-Cuperlovic, Ciriaco Piccirillo, Jörg Fritz
Partner institutions: The Ottawa Hospital, University of Ottawa, McGill University, National Research Council, Ottawa Methods Centre
Study website: https://omc.ohri.ca/SSO/
Global impact of COVID-19 research at The Ottawa Hospital
Since the start of the pandemic, researchers at The Ottawa Hospital have led or contributed to more than COVID-19 studies, including 25 clinical trials. Many of these studies have had an impact around the world.
“I want to thank all the patients and volunteers who have contributed to COVID-19 research, both by participating in studies and by helping to design them,” said Dr. Stewart. “I also want to thank all the generous donors who contributed to our COVID-19 Emergency Response Fund, which provided crucial seed funding to get many of our research projects off the ground.”
The Ottawa Hospital’s Ottawa Methods Centre is also playing an important role in many of the hospital’s COVID-19 studies, including the four new studies funded by the COVID-19 Immunity Task Force.
About The Ottawa Hospital
The Ottawa Hospital is one of Canada’s top learning and research hospitals, where excellent care is inspired by research and driven by compassion. As the third-largest employer in Ottawa, our support staff, researchers, nurses, physicians, and volunteers never stop seeking solutions to the most complex health-care challenges. Our multi-campus hospital, affiliated with the University of Ottawa, attracts some of the most influential scientific minds from around the world. Backed by generous support from the community, we are committed to providing the world-class, compassionate care we would want for our loved ones. www.ohri.ca
Media Contact
Jenn Ganton
613-614-5253
jganton@ohri.ca
