Newsroom
Deep-brain stimulation brings a family doctor with Parkinson’s back from “the abyss”
June 30, 2015
 Doctors aren’t known for their great handwriting skills, but this was more than just bad handwriting. Dr. Jacques Theriault’s writing got smaller as he moved across the page. It was 2006 when he first noticed the problem, and while most people might think nothing of it, Dr. Theriault, a family doctor, suspected it was a symptom of Parkinson’s.
Doctors aren’t known for their great handwriting skills, but this was more than just bad handwriting. Dr. Jacques Theriault’s writing got smaller as he moved across the page. It was 2006 when he first noticed the problem, and while most people might think nothing of it, Dr. Theriault, a family doctor, suspected it was a symptom of Parkinson’s.
His diagnosis was soon confirmed, and his disease eventually progressed to the point that he was taking 19 pills a day, with serious side effects. Although the pills helped control the symptoms for a while, eventually they stopped working and the tremors became unbearable.
“I was on the edge of an abyss,” he said. “I was going to end up in a wheelchair.”
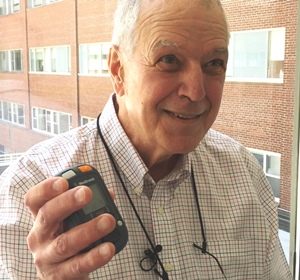
Everything changed in late 2014 when Dr. Theriault became one of the first people in Ottawa to be treated with deep-brain stimulation. The procedure, previously available only in Toronto for Ottawa-area patients, involves implanting electrodes into the brain, and connecting them to a stimulator implanted in the chest. The system provides regular electrical pulses to certain areas of the brain and has been proven to help control Parkinson’s symptoms in patients for whom other therapies have failed. The Ottawa Hospital recently obtained Ontario government funding to perform one deep-brain stimulation procedure per month.
“After the procedure I immediately felt better,” said Dr. Theriault. “I gradually reduced my medication and now I’m not taking any pills at all. I still sometimes have slow movements and problems with balance, but I’m 100 percent better.”
Dr. Adam Sachs hopes to develop a more customized and responsive form of deep-brain stimulation.
Dr. Adam Sachs, the neurosurgeon who performed the procedure at The Ottawa Hospital, noted that, while deep-brain stimulation works for some people, it may not work for everyone and the benefits can vary. That’s why he’s doing research to try to understand and improve the procedure. In fact, Dr. Theriault participated in a research study during his full-day surgery, wearing 3D goggles and using only his brain to manipulate objects in virtual reality.
“Deep-brain stimulation sends constant signals to the brain throughout the day, but Parkinson’s symptoms aren’t constant,” said Dr. Sachs, who is also a professor at the University of Ottawa. “Our experiments could help us develop a more responsive and customized type of deep-brain stimulation, and could perhaps even teach patients to focus their own brain activity to help control their symptoms.”
When asked to participate in the study, Dr. Theriault never hesitated.
For further information, please contact
Lois Ross
Senior Communications Specialist
Ottawa Hospital Research Institute
Office: 613-737-8899 x73687
Cell: 613-297-8315
loross@ohri.ca
