Abnormal electrolyte levels in people with eating disorders may increase risk of death, poor health outcomes
 "These findings underscore the importance of testing for electrolyte levels in people suffering from eating disorders, and then acting on those results to potentially reduce the risk of death or other severe outcomes," - Dr. Nicholas FabianoA new study published in The Lancet Psychiatry found that 32% of individuals with an eating disorder had abnormal electrolyte levels, which were associated with a higher risk of death from any cause.
"These findings underscore the importance of testing for electrolyte levels in people suffering from eating disorders, and then acting on those results to potentially reduce the risk of death or other severe outcomes," - Dr. Nicholas FabianoA new study published in The Lancet Psychiatry found that 32% of individuals with an eating disorder had abnormal electrolyte levels, which were associated with a higher risk of death from any cause.
The study, led by researchers at The Ottawa Hospital and ICES, found that electrolyte abnormalities were also linked to the development of other serious health conditions, including chronic kidney disease, bone fracture, bowel obstruction, and acute kidney injury.
This is one of the first large, population-based studies to identify an important risk factor for mortality and poor health outcomes in individuals suffering from eating disorders. Electrolytes, such as potassium and sodium, can affect how the body functions. It's common to find that people with eating disorders have electrolyte abnormalities due to symptoms such as purging, the use of laxatives, and dehydration.
"These findings might inform explicit mention of electrolyte abnormalities in the criteria we use to assess the severity of eating disorders," says lead author Dr. Marco Solmi, Medical Director of the Regional Eating Disorder Program at The Ottawa Hospital, and Director of research at the University of Ottawa's Psychiatry Department.
The researchers included over 6,000 individuals 13 years of age and older who were diagnosed with an eating disorder and had an electrolyte level test within one year of their diagnosis, as recorded on a hospitalization or emergency department record in the province of Ontario, Canada.
Health outcomes and mortality
Analyzing health records between 2008 and 2019, the researchers found that:
- Most people included in the study were diagnosed with an eating disorder not otherwise specified--disordered eating that falls outside the criteria for anorexia, bulimia and binge eating (59%) -- followed by anorexia nervosa (22%) and bulimia nervosa (15%).
- The mean age was 27 years, and 89% were female.
- 1,987 individuals (32%) had an electrolyte abnormality, and many had co-occurring health conditions.
- Among those with an electrolyte disorder, 16% died compared to 6% in those without an electrolyte abnormality.
- Electrolyte abnormalities were also associated with a higher risk of hospitalization and other serious health conditions, but not with a risk of infection or heart disease event.
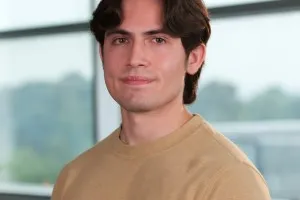
"These findings underscore the importance of testing for electrolyte levels in people suffering from eating disorders, and then acting on those results to potentially reduce the risk of death or other severe outcomes," says co-lead author Dr. Nicholas Fabiano, a psychiatry resident at The Ottawa Hospital and the University of Ottawa.
There is also a role for patient education and awareness. "Eating disorders are conditions that patients may often deny the existence of, or patients fail to appreciate the implications to their health. This study now shows that eating disorders which are severe enough to cause electrolyte disturbances have major ramifications in regard to long-term patient health outcomes," says senior author Dr. Gregory Hundemer, adjunct scientist at ICES, nephrologist and Lorna Jocelyn Wood Chair for Kidney Research at The Ottawa Hospital, and assistant professor at the University of Ottawa.
Finally, the researchers suggest that the findings can help to redefine how clinicians score the severity of eating disorders, which is currently based on a patient's body mass index and the frequency of behaviours like binge episodes. Electrolyte abnormalities may be found in patients who do not fit more typical eating disorder presentations and could ultimately help improve care for these patients and reduce their risk of death or other negative outcomes.
The article "Adverse outcomes and mortality in individuals with eating disorder-related electrolyte abnormalities: a population-based cohort study in Ontario, Canada" was published in The Lancet Psychiatry.
ICES is an independent, not-for-profit research and analytics institute that uses population-based health information to produce knowledge on a broad range of healthcare issues. ICES leads cutting-edge studies and analyses evaluating healthcare policy, delivery, and population outcomes. Our knowledge is highly regarded in Canada and abroad and is widely used by government, hospitals, planners, and practitioners to make decisions about healthcare delivery and to develop policy. For the latest ICES news, follow us on X, formerly Twitter: @ICESOntario
The Ottawa Hospital (TOH) is one of Canada's top learning and research hospitals where we are guided by our vision to provide the world-class and compassionate care we would all want for our loved ones. Our multi-campus hospital, affiliated with the University of Ottawa, is home to the Regional Trauma Centre and Cancer Centre, and to discoveries that are adopted globally. Backed by generous support from the community, we are focused on reshaping the future of health care to improve the health of our diverse population of patients from Eastern Ontario, Western Quebec, and Nunavut. For more information about The Ottawa Hospital, visit OttawaHospital.on.ca.
The University of Ottawa is home to over 50,000 students, faculty and staff, who live, work and study in both French and English. Our campus is a crossroads of cultures and ideas, where bold minds come together to inspire game-changing ideas. We are one of Canada's top 10 research universities--our professors and researchers explore new approaches to today's challenges. One of a handful of Canadian universities ranked among the top 200 in the world, we attract exceptional thinkers and welcome diverse perspectives from across the globe. www.uottawa.ca
FOR FURTHER INFORMATION PLEASE CONTACT:
Misty Pratt
Senior Communications Associate, ICES
Learn more about:
The Ottawa Hospital is a leading academic health, research and learning hospital proudly affiliated with the University of Ottawa and supported by The Ottawa Hospital Foundation.