11 big ideas to transform patient care and develop new treatments: ELEVATE competition results
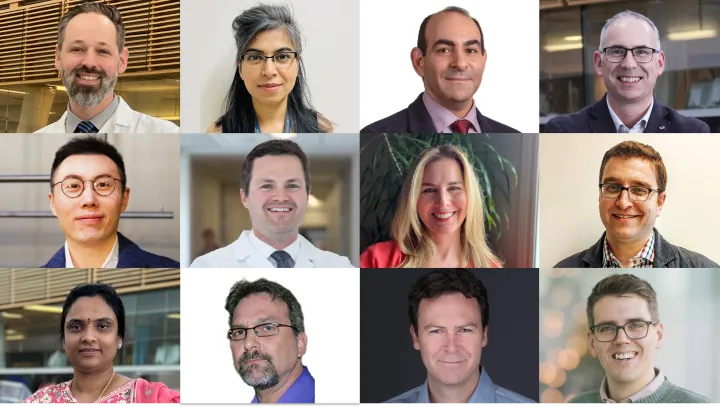
The Ottawa Hospital Research Institute (OHRI) is awarding 11 ELEVATE seed grants to kickstart innovative research projects that could improve patient care and lead to new treatments.
This year’s grants are focused on conditions such as liver disease, kidney disease, joint infections, breast cancer, trauma, neuroimmune disease, diabetes, chronic pain and mental health.
ELEVATE is funded in part by gifts to OHRI through The Ottawa Hospital Foundation. Applications are reviewed by a panel of internal and external researchers as well as patient partners. More than $400,000 was awarded through three ELEVATE streams this year.
“OHRI’s ELEVATE competition provides critical seed funding to help our research teams advance original and creative ideas to improve health and patient care,” said Dr. Rebecca Auer, Executive Vice-President of Research and Innovation, The Ottawa Hospital, CEO and Scientific Director, Ottawa Hospital Research Institute. “Many of our ELEVATE grant recipients have gone on to receive larger external grants and our patients are continuing to benefit from these research projects.”
Interprofessional research grants stream
This stream supports early-stage research projects led by allied health and nursing professionals as part of a partnership with The Ottawa Hospital’s INSPIRE Interprofessional Research Community of Practice. The projects must have clear potential to improve patient safety, quality of care and health outcomes.
Three grants were awarded in this stream:
Team research grants stream
This stream is designed to catalyze new research collaborations across a broad range of disease areas, providing teams with seed funding to kickstart innovative projects and obtain preliminary data for larger external grant applications.
Five grants were awarded in this stream:
Kidney research team grants stream
This stream is designed to catalyze new research collaborations related to kidney disease, providing teams with seed funding to kickstart innovative projects and obtain preliminary data for larger external grant applications.
Three grants were awarded in this stream:
Learn more about:
- Methodological and Implementation Research Program
- Acute Care Research Program
- Neuroscience Program
- Cancer Research Program
- Regenerative Medicine Program
- Inflammation and Chronic Disease Program
- Diabetes
- Type 1 diabetes
- Mental health
- Chronic pain
- Liver disease
- Infectious disease
- Breast cancer
- Traumatic injuries
- Brain and neuromuscular disease
- Autoimmune disease
- Kidney disease
- Vascular, heart and metabolic disease
- Clinical research
- Qualitative methods
- Patient engagement
- Patient safety
- Quality Improvement
- Health services research
- Disease models
- Molecular and cellular biology
- Transgenic/knockout models
- Stem cells
- Genetics
- Viral therapy
- Infectious disease
- Drug development
- Rehabilitation
- Transplantation
- Surgery
- Biomaterials
- Drug development
- Critical care
The Ottawa Hospital is a leading academic health, research and learning hospital proudly affiliated with the University of Ottawa and supported by The Ottawa Hospital Foundation.


